Hi!
I am currently modelling the processes in an Emergency Department - in part for work, in part for a master’s thesis in information systems.
My focus at this point is the triage process. In Germany two of these are dominant, the Manchester Triage System (MTS) and to some extent the Harvard-born Emergency Severity Index (ESI).
The latter, unfortunately, is the one favored by my local ED director. Unfortunate because the ESI “algorithm” isn’t that easy to grasp (MTS is much more linear).
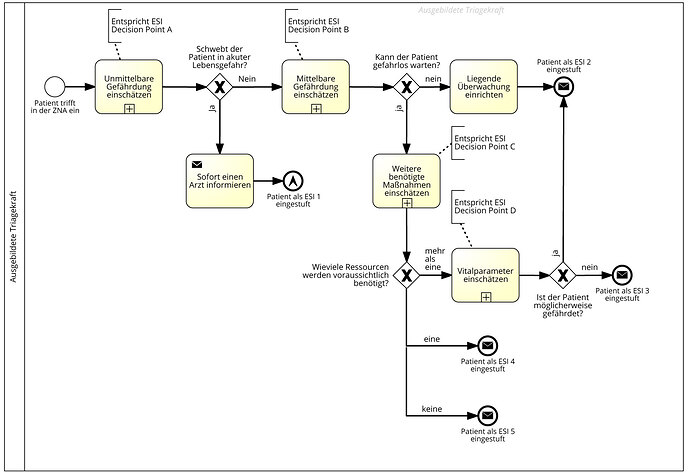
On a strategic level it is easy enough to do in BPMN:
You first see whether a patient needs immediate care, if yes, you escalate immediately (basically you raise an alarm). If not, you need to decide whether the condition can escalate to a life-threatening point in the very near future (30 minutes or so). If that is not the case, you estimate how many ressources (x-rays, CT, ECG, lab runs, etc.) the patient’s treatment is going to require, if it is more than one you classify in group 3, one in group 4, and none in group 5.
If you classify in group 3, you also look at the basic vital parameters and if there is something “fishy” there, you escalate that patient back to 2 (which means a physician has to look at that patient within 15 minutes).
In more detail:
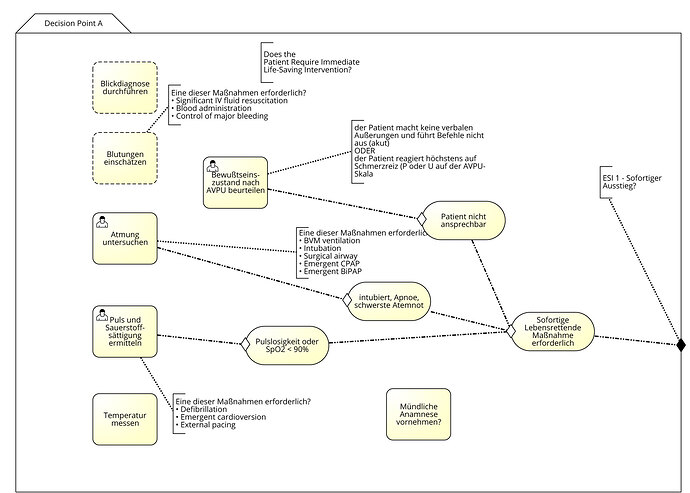
At decision point A the experienced triage nurse (which is mandatory for the process) is supposed to ask “Does the patient require immediate life-saving interventions?”. Unfortunately the process doesn’t tell you exactly how to gain the information to answer that question.
The basic procedures at this point of course may depend on what is immediately obvious: arterial bleeding, unconsciousness, etc. Some things may raise alarms when the patient mentions certain keywords (for example chest pain or numbness in the arm, or a hard abdomen with a patient slapping a hand away that tries to touch it).
In ESI there is no real procedure for this apart from “needing an experienced nurse”. So as a first step I modelled this in CMMN:
Items that are definitely checked are breathing “Atmung untersuchen”, pulse and O2 saturation, temperature and whether the patient is able to communicate with you (level of consciousness, basically AVPU stands for the Alert, Voice, Pain, Unresponsive scale).
In a second step (decision Point B), the question to answer is: “Would you give this patient your last bed?”.
Here once again the experience is key: Does the triage nurse “see” things that tell him/her something is wrong? Is the reported pain level (“Schmerz-Score”) or distress level very high? Does the patient appear disoriented, lethargic or confused? This once again I find very difficult to model (and don’t dare post the current state of my DP B model ;-)).
Now - do you have any suggestions on how to improve the modelling at this stage? I found it quite hard to find more complex examples/best practices to learn something from. Most examples I found deal with quite simple cases.
I’ll very much appreciate any input I can get here!